The Relationship Between Stress and Diabetes
When your body experiences stress, it triggers what’s known as the “fight-or-flight” response. This evolutionary mechanism releases hormones like adrenaline and cortisol into your bloodstream. While this response was helpful for our ancestors facing physical threats, today’s chronic stress can have damaging effects on blood glucose regulation.
During stress, your body releases glucose into the bloodstream to provide energy for dealing with the perceived threat. For people without diabetes, the pancreas typically produces enough insulin to manage this temporary rise. However, when stress becomes chronic, this system can become overwhelmed.
According to research from Harvard Medical School, prolonged stress can contribute to insulin resistance, where cells become less responsive to insulin’s effects. This forces the pancreas to work harder to produce more insulin, potentially leading to pancreatic fatigue over time.
“Chronic stress creates a perfect storm of conditions that can contribute to diabetes development. The constant elevation of stress hormones makes it increasingly difficult for insulin to do its job effectively.”
Studies show that people in high-stress occupations have approximately a 30% increased risk of developing type 2 diabetes compared to those in lower-stress jobs. This connection appears strongest in individuals who also have other risk factors for diabetes.
Biological Mechanisms: How Stress Affects Blood Sugar
The connection between stress and diabetes involves several biological mechanisms:
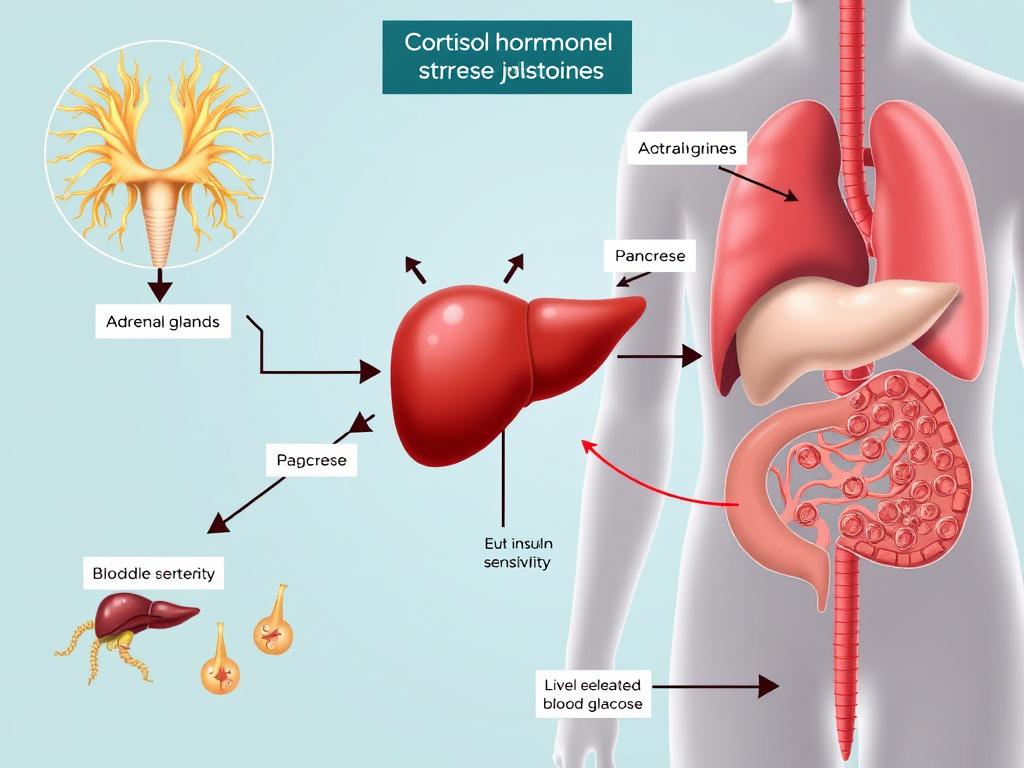
Cortisol’s Role in Insulin Resistance
Cortisol, often called the “stress hormone,” plays a central role in this relationship. When chronically elevated, cortisol:
- Increases glucose production in the liver
- Reduces insulin sensitivity in muscle and fat cells
- Promotes visceral fat accumulation, which further contributes to insulin resistance
- Interferes with insulin production in the pancreas
Inflammatory Response
Chronic stress triggers low-grade inflammation throughout the body. This inflammatory state:
- Damages insulin-producing beta cells in the pancreas
- Creates additional insulin resistance in tissues
- Disrupts normal glucose metabolism pathways
- Accelerates complications in existing diabetes
A study published in the Journal of Endocrinology found that participants exposed to chronic psychological stress showed a 60% increase in insulin resistance compared to control groups. This demonstrates how powerfully stress can impact your body’s ability to regulate blood sugar.
Want to understand your stress response better?
Take our free stress assessment quiz to identify your personal stress triggers and learn tailored management techniques.
How Stress Affects Different Types of Diabetes
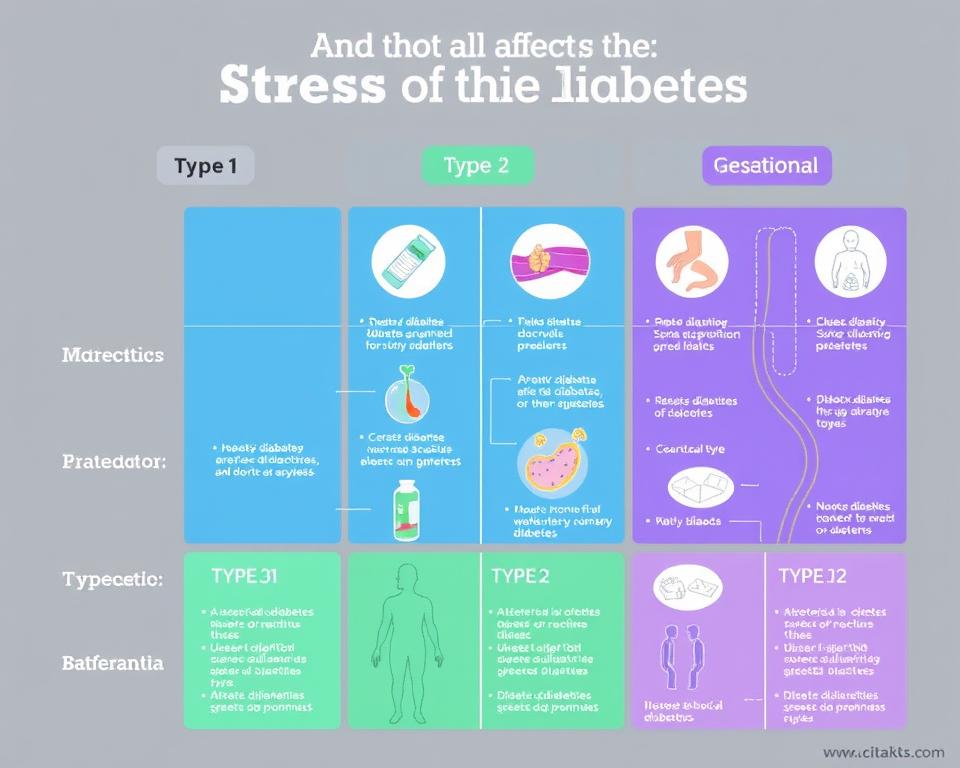
Type 1 Diabetes
While stress doesn’t directly cause Type 1 diabetes (an autoimmune condition), research suggests it may:
- Trigger or accelerate the autoimmune response in genetically susceptible individuals
- Make blood glucose management more difficult for those already diagnosed
- Increase the frequency of hyperglycemic episodes
Type 2 Diabetes
The relationship between stress and Type 2 diabetes is more direct:
- Chronic stress contributes to insulin resistance, a primary factor in Type 2 development
- Stress often leads to unhealthy coping behaviors (poor diet, reduced exercise) that increase risk
- Stress-related weight gain, especially around the abdomen, significantly raises diabetes risk
Gestational Diabetes
Pregnant women experiencing high stress levels may face:
- Increased risk of developing gestational diabetes
- More difficulty managing blood glucose during pregnancy
- Higher likelihood of complications for both mother and baby
- Greater chance of developing Type 2 diabetes later in life
A longitudinal study following over 10,000 women found that those reporting high levels of work-related stress had a 45% higher risk of developing gestational diabetes compared to women with lower stress levels.
Debunking Myths: What Science Really Says
Facts
- Chronic stress is a significant risk factor for developing Type 2 diabetes
- Stress management can improve blood glucose control in people with diabetes
- The stress-diabetes connection is supported by multiple peer-reviewed studies
- Biological mechanisms linking stress and diabetes are well-documented
Myths
- Stress alone causes diabetes (false – multiple factors are involved)
- All types of diabetes are equally affected by stress (false – effects vary by type)
- Short-term stress is as harmful as chronic stress (false – duration matters)
- Stress management alone can cure diabetes (false – comprehensive management is needed)
It’s important to understand that while stress is a significant factor in diabetes risk, it’s rarely the sole cause. Genetic predisposition, lifestyle factors, and environmental influences all play important roles. However, stress management represents one of the most accessible ways to potentially reduce your risk.
Important: If you’re experiencing symptoms of diabetes (increased thirst, frequent urination, unexplained weight loss, fatigue), consult a healthcare provider regardless of your stress levels. Early diagnosis and treatment are essential for preventing complications.
Effective Stress Management Strategies to Reduce Diabetes Risk

Managing stress effectively may help reduce your risk of developing diabetes or improve management if you already have the condition. Here are evidence-based strategies:
Physical Techniques
- Regular exercise: 30 minutes of moderate activity 5 days a week can reduce stress hormones by up to 25%
- Deep breathing: Practice 4-7-8 breathing (inhale for 4, hold for 7, exhale for 8) to activate the parasympathetic nervous system
- Progressive muscle relaxation: Systematically tense and release muscle groups to reduce physical tension
- Adequate sleep: Aim for 7-9 hours of quality sleep to regulate stress hormones
Mental Techniques
- Mindfulness meditation: Studies show 10 minutes daily can reduce cortisol levels by up to 20%
- Cognitive restructuring: Identify and challenge negative thought patterns that contribute to stress
- Guided imagery: Visualize peaceful scenes to activate relaxation response
- Journaling: Write about stressors to process emotions and gain perspective
Lifestyle Adjustments
- Balanced nutrition: Emphasize whole foods that stabilize blood sugar and support stress response
- Social connection: Maintain supportive relationships that buffer against stress effects
- Time management: Set realistic goals and boundaries to reduce overwhelm
- Nature exposure: Spend time outdoors to reduce cortisol and improve mood
Research published in the journal Diabetes Care found that participants who completed an 8-week stress management program showed significant improvements in both stress levels and glycemic control compared to control groups.
Ready to reduce your stress and diabetes risk?
Download our comprehensive guide with 30-day stress reduction plan specifically designed for diabetes prevention.
Frequently Asked Questions About Stress and Diabetes

Can a single stressful event cause diabetes?
A single stressful event is unlikely to cause diabetes in someone without pre-existing risk factors. However, extremely traumatic events that lead to prolonged stress responses might contribute to diabetes development in susceptible individuals. Research shows that people who experience severe trauma have a 13% higher risk of developing type 2 diabetes over the following 5 years.
How quickly can stress affect blood sugar levels?
Stress can affect blood sugar levels almost immediately. Within minutes of experiencing acute stress, stress hormones can cause blood glucose to rise. For people with diabetes, this effect can be particularly pronounced, sometimes raising blood sugar by 30-40 mg/dL within 30 minutes of a stressful event. This is why stress management is an important component of diabetes care.
Are some people more susceptible to stress-induced blood sugar changes?
Yes, sensitivity to stress-induced blood sugar changes varies significantly between individuals. Factors that increase susceptibility include family history of diabetes, existing insulin resistance, obesity (particularly abdominal fat), poor sleep habits, and certain genetic variations. People with these risk factors may benefit most from proactive stress management.
Can stress management reverse prediabetes?
While stress management alone may not completely reverse prediabetes, it can be an important part of a comprehensive approach. Studies show that combining stress reduction techniques with dietary changes and increased physical activity can help normalize blood glucose levels in prediabetic individuals. A study in the New England Journal of Medicine found that lifestyle interventions including stress management reduced progression to diabetes by 58% in high-risk individuals.
If you’re concerned about prediabetes, learn more about comprehensive prevention strategies.
Taking Control: Your Next Steps

The connection between stress and diabetes is complex but increasingly well-understood. While stress alone doesn’t cause diabetes, chronic stress creates physiological conditions that can increase your risk, particularly when combined with other factors like genetics, diet, and activity level.
The good news is that stress management represents one of the most accessible ways to potentially reduce your diabetes risk. By incorporating the strategies outlined in this article, you can take meaningful steps toward better health.
Remember that managing stress is just one component of diabetes prevention. A holistic approach that includes regular physical activity, balanced nutrition, adequate sleep, and regular medical check-ups provides the strongest protection against diabetes development.
Ready for personalized support?
Download our comprehensive stress management guide specifically designed for diabetes prevention. This 30-page resource includes stress assessment tools, a 4-week stress reduction plan, and expert advice from endocrinologists.


