Understanding High Blood Pressure
Blood pressure is the force exerted against your artery walls as your heart pumps blood throughout your body. It’s measured in millimeters of mercury (mm Hg) and recorded as two numbers: systolic pressure (when your heart beats) over diastolic pressure (when your heart rests between beats).
| Blood Pressure Category | Systolic (mm Hg) | Diastolic (mm Hg) |
| Normal | Less than 120 | Less than 80 |
| Elevated | 120-129 | Less than 80 |
| Stage 1 Hypertension | 130-139 | 80-89 |
| Stage 2 Hypertension | 140 or higher | 90 or higher |
| Hypertensive Crisis | Higher than 180 | Higher than 120 |
According to the American Heart Association, nearly half of American adults have high blood pressure, and many don’t even know it. That’s why hypertension is often called the “silent killer” – it typically has no symptoms until significant damage has already occurred.

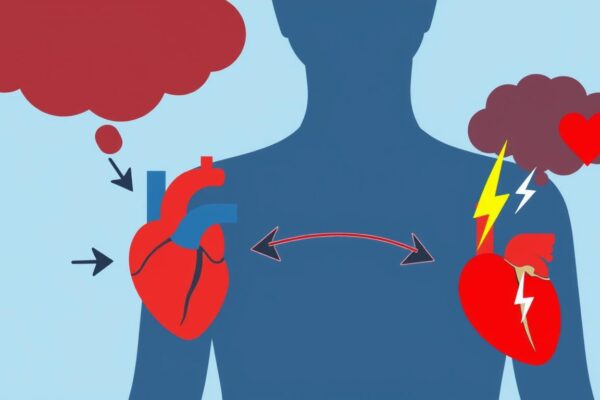
The Physiological Connection: How High Blood Pressure Damages Your Heart
High blood pressure doesn’t cause heart disease overnight. Instead, it creates a cascade of damaging effects that unfold over years. Understanding these mechanisms helps explain why controlling blood pressure is so crucial for heart health.
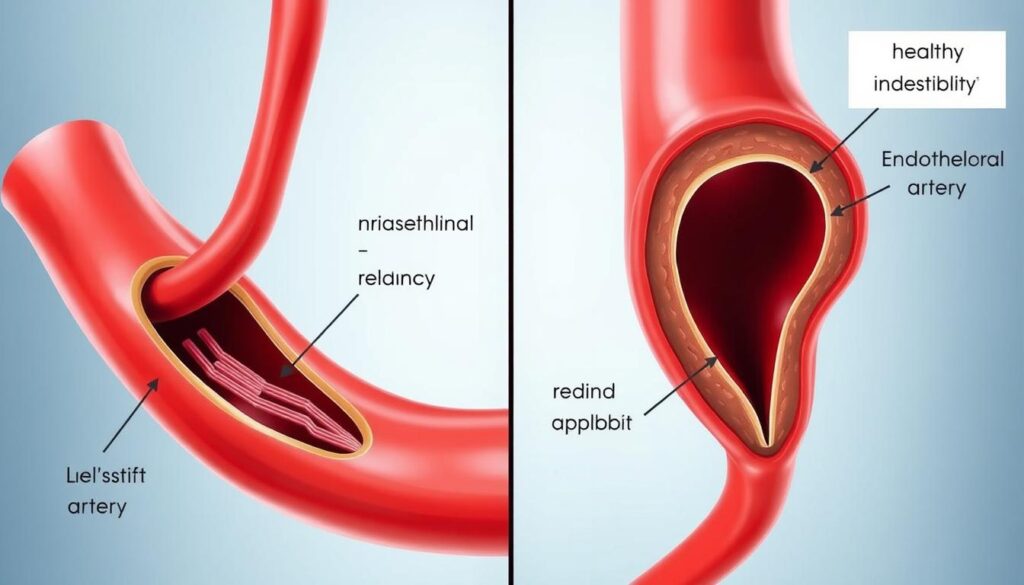
Arterial Damage and Stiffening
Your arteries are designed to be elastic, expanding and contracting with each heartbeat. When blood pressure remains consistently high, it forces your arteries to work harder, causing several problems:
- The inner lining of arteries (endothelium) becomes damaged
- Arteries lose elasticity and become stiff
- Blood flow becomes restricted
- Oxygen delivery to organs decreases
Increased Heart Workload
When arteries stiffen and narrow, your heart must work harder to pump blood through them. This increased workload leads to:
- Enlargement of the heart muscle (left ventricular hypertrophy)
- Thickening of heart walls
- Reduced pumping efficiency
- Increased oxygen demand by the heart muscle
Over time, this extra strain can weaken your heart and lead to heart failure, where the heart can’t pump enough blood to meet your body’s needs.
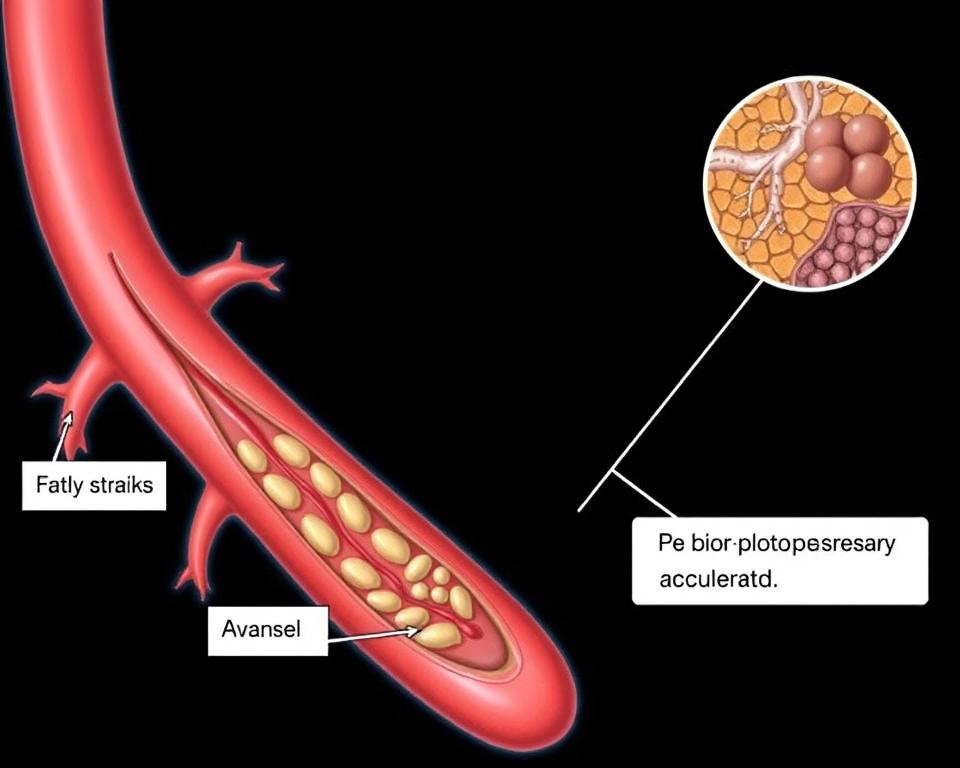
Accelerated Atherosclerosis
High blood pressure accelerates the development of atherosclerosis – the buildup of fatty plaques in your arteries. This happens because:
- Damaged artery walls are more prone to cholesterol and fat deposits
- Inflammation increases in damaged areas
- Plaques form and grow, narrowing arteries
- Blood clots are more likely to form on plaque surfaces
Learn More About Your Heart Health
Understanding your blood pressure numbers is the first step toward better heart health. The American Heart Association offers resources to help you track and manage your blood pressure.
Risk Factors That Amplify the Connection
Certain factors can strengthen the link between high blood pressure and heart disease, accelerating damage and increasing your risk of serious complications. Understanding these factors can help you identify your personal risk level.
Modifiable Risk Factors
- Obesity – Excess weight increases blood volume and creates more resistance in your blood vessels
- Sedentary lifestyle – Lack of physical activity weakens your heart and blood vessels
- High sodium diet – Excess salt causes fluid retention and increases blood volume
- Tobacco use – Smoking damages blood vessels and raises blood pressure
- Excessive alcohol – Regular heavy drinking raises blood pressure and damages heart muscle
- Chronic stress – Persistent stress hormones constrict blood vessels and raise blood pressure
Non-Modifiable Risk Factors
- Age – Blood vessels naturally stiffen with age
- Family history – Genetic factors influence blood pressure regulation
- Race – African Americans have higher rates of severe hypertension
- Gender – Men have higher risk until age 65, then women’s risk increases
- Chronic kidney disease – Kidney problems affect blood pressure regulation

Compounding Effects
When multiple risk factors are present, they don’t just add to your risk – they multiply it. For example, having both high blood pressure and diabetes increases your risk of heart disease far more than either condition alone. According to the American Heart Association, when high blood pressure combines with obesity, the risk of heart failure increases by 75%.
Effective Prevention Strategies
The good news is that you can take control of your blood pressure and significantly reduce your risk of heart disease. Research shows that even small improvements in blood pressure can lead to major reductions in heart disease risk.
Dietary Approaches
What you eat has a powerful effect on your blood pressure. The DASH diet (Dietary Approaches to Stop Hypertension) has been proven to lower blood pressure within weeks.
- Reduce sodium – Aim for less than 2,300mg daily (about 1 teaspoon of salt)
- Increase potassium – Eat bananas, potatoes, avocados, and leafy greens
- Limit processed foods – They often contain hidden sodium
- Eat more fruits and vegetables – Aim for 8-10 servings daily
- Choose whole grains – They provide fiber and nutrients that support heart health
- Limit alcohol – No more than 1 drink daily for women, 2 for men

Physical Activity
Regular exercise strengthens your heart and improves blood vessel function. The American Heart Association recommends:
- At least 150 minutes of moderate-intensity aerobic activity weekly
- Muscle-strengthening activities at least twice weekly
- Breaking up sitting time with short activity breaks
- Starting slowly if you’ve been inactive and gradually increasing intensity
“For most people, a 5-10 mm Hg reduction in blood pressure can be achieved through regular physical activity – the equivalent benefit of some prescription medications.”
Medication Adherence
If your doctor prescribes blood pressure medication, taking it as directed is crucial. Studies show that:
- 50% of patients stop taking blood pressure medications within one year
- Non-adherence accounts for approximately 125,000 deaths annually
- Proper medication use can reduce heart attack risk by 20-25%

Track Your Blood Pressure at Home
Regular monitoring is key to managing blood pressure. Home monitoring helps you and your doctor see how well your treatment plan is working.
Stress Management
Chronic stress contributes to high blood pressure and heart disease. Effective stress management techniques include:
- Meditation and mindfulness practices
- Deep breathing exercises
- Regular physical activity
- Adequate sleep (7-8 hours nightly)
- Social connection and support
- Professional counseling when needed

When to Consult Your Doctor
Regular blood pressure monitoring is essential, but certain situations warrant immediate medical attention. Contact your healthcare provider if:
- Your blood pressure readings consistently exceed 130/80 mm Hg
- You experience significant changes in blood pressure
- You have difficulty controlling your blood pressure despite following your treatment plan
- You experience side effects from blood pressure medications
Seek emergency care immediately if your blood pressure exceeds 180/120 mm Hg, especially if accompanied by chest pain, severe headache, vision problems, or difficulty breathing.

Talk to Your Doctor About Your Heart Health
Regular checkups are essential for monitoring your blood pressure and heart health. Don’t wait until symptoms appear – early intervention saves lives.
Blood Pressure Monitoring Tools
Home monitoring is a crucial part of managing high blood pressure. Regular readings help you and your doctor determine if your treatment plan is working effectively.
Choosing a Blood Pressure Monitor
Recommended Features:
- Automatic operation with digital display
- Upper arm cuff (more accurate than wrist models)
- Proper cuff size for your arm
- Memory storage for previous readings
- Validation by medical organizations
Using Your Monitor Correctly:
- Measure at the same time each day
- Avoid caffeine, exercise, and smoking for 30 minutes prior
- Sit with back supported and feet flat on floor
- Rest arm at heart level on a flat surface
- Take multiple readings and record results

Tracking Tip: Many smartphone apps can help you track blood pressure readings over time. These digital tools make it easy to share your results with your healthcare provider and identify patterns that might otherwise go unnoticed.
Frequently Asked Questions
Can lowering blood pressure reverse heart damage?
Yes, to some extent. While certain types of heart damage may be permanent, research shows that controlling blood pressure can significantly improve heart function and prevent further damage. The heart has remarkable ability to recover when blood pressure is maintained at healthy levels.
Studies show that for every 10 mm Hg reduction in systolic blood pressure, the risk of heart failure decreases by about 28%. Even if you’ve had high blood pressure for years, bringing it under control now can still benefit your heart health.
What blood pressure range is considered dangerous?
Blood pressure readings above 180/120 mm Hg are considered a hypertensive crisis requiring immediate medical attention. However, any reading above 130/80 mm Hg (Stage 1 hypertension) increases your risk of heart disease and requires attention.
The risk of heart disease begins to rise at blood pressure levels above 115/75 mm Hg, and it doubles with each 20/10 mm Hg increase. This is why the American Heart Association recommends maintaining blood pressure below 120/80 mm Hg for optimal heart health.
How often should blood pressure be monitored?
Monitoring frequency depends on your current blood pressure status:
- For normal blood pressure (below 120/80 mm Hg): Check at least once every 2 years
- For elevated or Stage 1 hypertension: Check at least annually, or as recommended by your doctor
- For diagnosed hypertension: Check at home 1-2 times daily, at varying times
- When starting or changing medications: Monitor more frequently as advised by your healthcare provider
Keep a log of your readings to share with your healthcare provider during appointments. This helps them assess how well your treatment plan is working.

Taking Control of Your Heart Health
The connection between high blood pressure and heart disease is clear and well-established. Every day your blood pressure remains elevated, it continues to damage your cardiovascular system. But this doesn’t mean heart disease is inevitable.
By understanding how high blood pressure affects your heart, recognizing your personal risk factors, and implementing the prevention strategies outlined in this article, you can significantly reduce your risk of developing heart disease. Remember that even small improvements in blood pressure can lead to major benefits for your heart health.
Don’t wait for symptoms to appear – high blood pressure silently damages your body long before you feel its effects. Take action today by monitoring your blood pressure, discussing concerns with your healthcare provider, and making heart-healthy lifestyle changes.

Start Your Heart Health Journey Today
Take the first step toward better heart health by downloading the American Heart Association’s blood pressure tracking guide and discussing your numbers with your healthcare provider.