The landscape of cardiovascular innovation has expanded dramatically in the past decade, with several groundbreaking medications receiving FDA approval. From drugs that help the heart beat more efficiently to those that reduce inflammation and prevent dangerous plaque buildup, these new medications in heart care are transforming treatment options for patients with various cardiac conditions.
New medications are transforming treatment options for heart disease patients
Breakthrough New Medications in Heart Care
The field of cardiology has seen remarkable advancements with several new medications gaining FDA approval in recent years. These drugs work through novel mechanisms to address the complex pathophysiology of heart disease, offering benefits beyond what traditional treatments could achieve.
SGLT2 Inhibitors: Beyond Diabetes Treatment
Originally developed for diabetes management, sodium-glucose cotransporter-2 (SGLT2) inhibitors have emerged as game-changers in heart failure treatment. Medications like empagliflozin (Jardiance) and dapagliflozin (Farxiga) work by preventing the kidneys from reabsorbing sugar, allowing it to be excreted through urine.
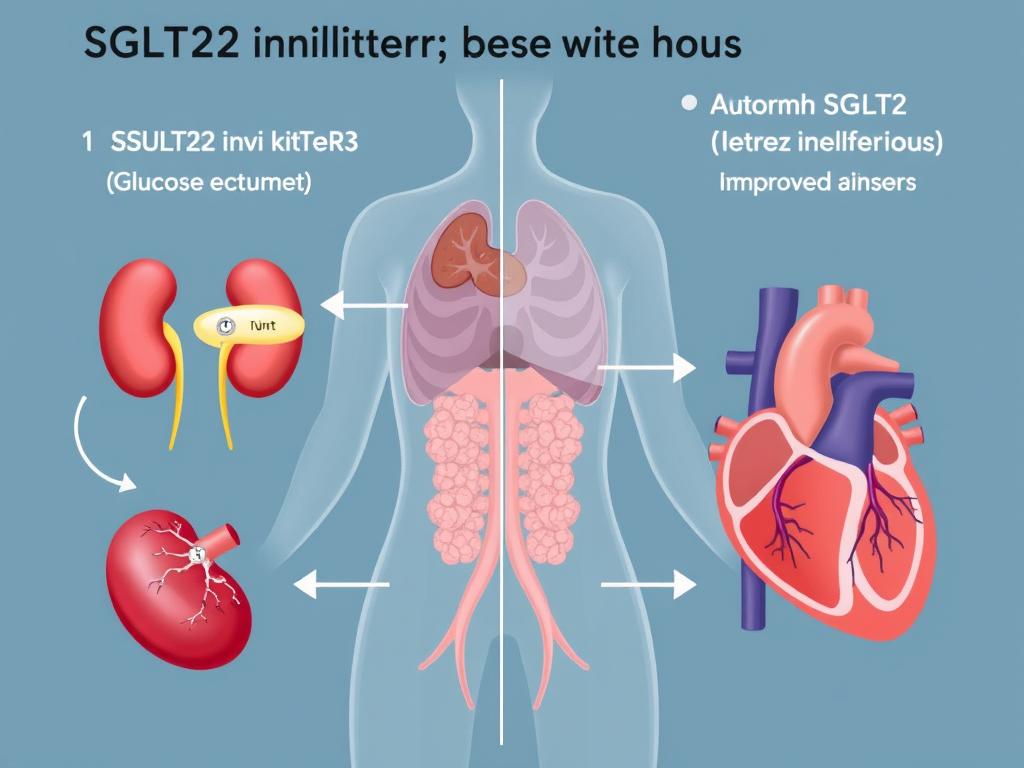
SGLT2 inhibitors prevent sugar reabsorption in the kidneys while providing heart benefits
Think of SGLT2 inhibitors as “sugar drain openers” – they allow excess glucose to leave the body rather than circulate in the bloodstream. What’s remarkable is that these medications have shown significant benefits for heart failure patients even without diabetes. Clinical trials have demonstrated a reduction in heart failure hospitalizations by up to 30% and improved survival rates.
Research has shown these medications can also help control other factors for cardiovascular disease, including lowering blood pressure, reducing inflammation, and improving the function of blood vessel linings. Studies have shown that SGLT2 inhibitors can lower the risk of major cardiovascular events like heart attack or stroke by up to 20%.
PCSK9 Inhibitors: Revolutionary Cholesterol Management
For patients with stubbornly high LDL (“bad”) cholesterol despite taking statins, PCSK9 inhibitors like Repatha (evolocumab) and Praluent (alirocumab) offer a powerful alternative. These medications work by blocking the PCSK9 protein that breaks down LDL receptors in the liver.
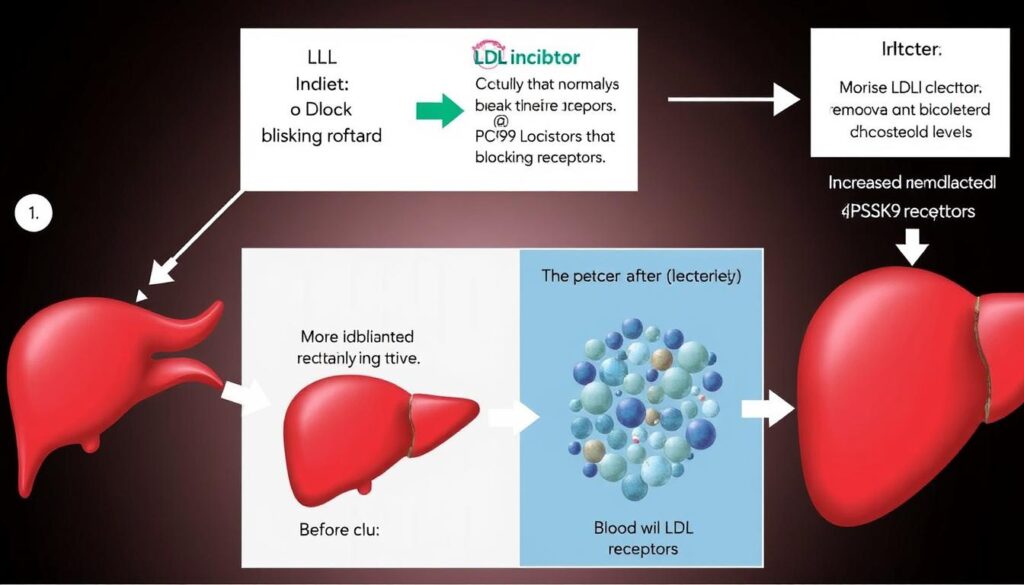
PCSK9 inhibitors prevent the breakdown of LDL receptors, allowing more cholesterol to be cleared from the bloodstream
To understand how PCSK9 inhibitors work, imagine your liver as a recycling center with special receptors that capture and remove LDL cholesterol from your blood. Normally, a protein called PCSK9 limits how many of these “recycling stations” are available. PCSK9 inhibitors block this limiting protein, allowing more recycling stations to remain active and remove more LDL from circulation.
These medications can reduce LDL cholesterol by an impressive 50-70%, far beyond what statins alone can achieve for many patients. This dramatic reduction helps prevent the buildup of artery-clogging plaque that can lead to heart attacks and strokes.
Sacubitril/Valsartan: Dual-Action Heart Failure Treatment
Sacubitril/valsartan (Entresto) represents the first in a new class of medications called angiotensin receptor-neprilysin inhibitors (ARNIs). This dual-action medication combines an angiotensin receptor blocker with a neprilysin inhibitor to address heart failure through two complementary mechanisms.
Sacubitril/valsartan works through two complementary mechanisms to improve heart function
The valsartan component blocks the harmful effects of the renin-angiotensin-aldosterone system, which can cause blood vessel constriction and fluid retention. Meanwhile, sacubitril enhances the body’s natural protective systems by preventing the breakdown of beneficial natriuretic peptides that promote vasodilation, diuresis, and reduced cardiac remodeling.
In the landmark PARADIGM-HF trial, sacubitril/valsartan reduced the risk of cardiovascular death or heart failure hospitalization by 20% compared to the previous standard of care. The medication also decreased all-cause mortality by 16% and slowed the decline in quality of life for heart failure patients.
Ivabradine: Heart Rate Control for Better Outcomes
Ivabradine (Corlanor) works through a unique mechanism that specifically targets the heart’s natural pacemaker, the sinoatrial node. By inhibiting the “funny” current (If) channels, ivabradine slows heart rate without the other cardiovascular effects of beta-blockers.
Ivabradine selectively slows heart rate by acting on the sinoatrial node
Think of ivabradine as a “tempo controller” for your heart. A faster heart rate increases the heart’s workload and oxygen demand. By specifically slowing the heart rate without affecting blood pressure or contractility, ivabradine reduces cardiac stress and improves efficiency.
Clinical trials have shown that ivabradine can reduce heart failure hospitalizations by 18% in patients with a resting heart rate above 70 beats per minute despite maximum tolerated doses of beta-blockers. This medication is particularly beneficial for patients who cannot tolerate high doses of beta-blockers due to side effects like fatigue or low blood pressure.
Vericiguat: Enhancing Heart Function Through Novel Pathways
Vericiguat (Verquvo) is the first soluble guanylate cyclase (sGC) stimulator approved for heart failure. This medication enhances the body’s nitric oxide-sGC-cyclic guanosine monophosphate (cGMP) pathway, which is often impaired in heart failure patients.
Vericiguat enhances the nitric oxide pathway to improve heart function and blood flow
By stimulating sGC, vericiguat increases the production of cGMP, which plays a crucial role in relaxing blood vessels and reducing the workload on the heart. This mechanism is particularly important in heart failure, where nitric oxide signaling is often diminished.
In the VICTORIA trial, vericiguat reduced the combined risk of cardiovascular death or heart failure hospitalization in patients with worsening heart failure. This medication provides a complementary approach to existing heart failure therapies and is particularly valuable for patients who have recently been hospitalized.
| Medication | Brand Name | Purpose | Key Benefit | Availability |
| SGLT2 Inhibitors (empagliflozin, dapagliflozin) | Jardiance, Farxiga | Heart failure treatment, diabetes management | 30% reduction in heart failure hospitalizations | FDA-approved, widely available |
| PCSK9 Inhibitors (evolocumab, alirocumab) | Repatha, Praluent | Advanced cholesterol management | 50-70% LDL cholesterol reduction | FDA-approved, prescription only |
| Sacubitril/Valsartan | Entresto | Heart failure with reduced ejection fraction | 20% reduction in cardiovascular death or hospitalization | FDA-approved, widely prescribed |
| Ivabradine | Corlanor | Heart rate reduction in heart failure | 18% reduction in heart failure hospitalizations | FDA-approved for specific patient groups |
| Vericiguat | Verquvo | Worsening heart failure treatment | Reduced risk of cardiovascular death or hospitalization | FDA-approved, newer to market |
Impact on Patients: Transforming Heart Care Outcomes
The introduction of these new medications has dramatically improved outcomes for heart disease patients. Statistical evidence from large clinical trials demonstrates their significant impact on reducing hospitalizations, improving quality of life, and extending survival.
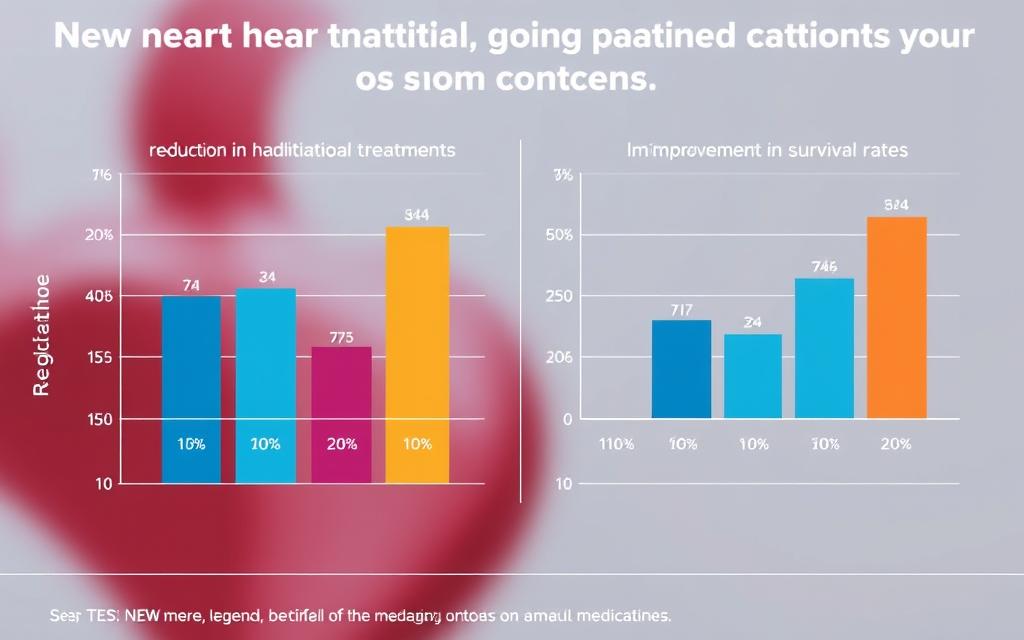
Clinical data showing the impact of new heart medications on hospitalization rates and survival
Reduced Hospitalizations and Improved Survival
The statistics tell a compelling story about the effectiveness of these new treatments:
- SGLT2 inhibitors have reduced heart failure hospitalizations by 25-30% in major clinical trials
- Sacubitril/valsartan has demonstrated a 20% reduction in cardiovascular death or heart failure hospitalization
- PCSK9 inhibitors have shown a 15-20% reduction in major adverse cardiovascular events in high-risk patients
- Combination therapy with multiple new medications can reduce two-year mortality by up to 50% and hospitalization risk by 64%
- Quality of life scores have improved significantly across multiple medication classes
Patient Success Story: Michael’s Journey
“After my second heart failure hospitalization in six months, my cardiologist prescribed a combination of sacubitril/valsartan and an SGLT2 inhibitor. The difference has been remarkable. My breathing has improved, I can walk up stairs without stopping, and I haven’t been back to the hospital in over a year. These new medications gave me my life back.”
Michael’s experience reflects what cardiologists are seeing across the country. Patients who previously cycled in and out of hospitals are now maintaining stable heart function and enjoying improved quality of life thanks to these innovative medications.

New heart medications are helping patients like Michael maintain better heart health
Expert Perspective on Treatment Evolution
“What’s truly revolutionary about these new medications is that they’re not just managing symptoms—they’re actually modifying the disease process itself. We’re seeing improvements in cardiac function, reductions in ventricular remodeling, and better outcomes across multiple patient populations. This is a paradigm shift in how we approach heart disease treatment.”
The real-world impact extends beyond individual patients. Healthcare systems are reporting decreased readmission rates for heart failure, reduced emergency department visits, and lower overall costs associated with cardiovascular care. This system-wide improvement demonstrates the broader economic and public health benefits of these innovative medications.
Challenges and Future of Heart Care Medications
Despite the remarkable advances in heart care medications, several challenges remain in ensuring these treatments reach all patients who could benefit from them.
Accessibility and Cost Considerations

Cost remains a significant barrier for many patients seeking access to new heart medications
Many of these breakthrough medications come with substantial price tags. PCSK9 inhibitors, for example, can cost several thousand dollars annually, while newer combination therapies may not be fully covered by all insurance plans. This creates disparities in access, with some patients unable to benefit from the latest advances in heart care.
Current Challenges
- High out-of-pocket costs for patients, even with insurance
- Prior authorization requirements creating treatment delays
- Limited coverage for newer medications
- Lack of awareness among patients and some providers
- Medication adherence issues due to cost and complexity
Emerging Solutions
- Patient assistance programs from pharmaceutical companies
- Value-based insurance designs that reduce costs for high-value medications
- Increased advocacy for broader insurance coverage
- Development of more affordable biosimilar versions
- Telehealth monitoring to improve medication adherence
Promising Medications in Clinical Trials
The pipeline for new heart medications continues to grow, with several promising candidates in late-stage clinical trials:

Researchers continue to develop the next generation of heart medications
Omecamtiv Mecarbil
This novel cardiac myosin activator works by increasing the duration of cardiac muscle contraction without increasing cellular calcium, potentially improving cardiac output without the oxygen demand increase seen with traditional inotropes. In the GALACTIC-HF trial, omecamtiv mecarbil showed promising results for patients with heart failure with reduced ejection fraction, particularly those with more severe disease.
Mavacamten
For patients with hypertrophic cardiomyopathy, mavacamten represents a potential breakthrough. This first-in-class cardiac myosin inhibitor reduces excessive contractility of the heart muscle, addressing the underlying cause of obstruction in hypertrophic cardiomyopathy. Early clinical trials have shown improvements in exercise capacity, symptoms, and quality of life.
The future of heart care will likely involve more personalized medication approaches
Research is also advancing in several other areas, including anti-inflammatory therapies targeting the IL-1β pathway, gene therapies for inherited cardiomyopathies, and novel approaches to heart failure with preserved ejection fraction, a condition that has traditionally been difficult to treat effectively.
Conclusion: A New Era in Heart Care
The landscape of heart care has been fundamentally transformed by these new medications. What was once a field limited to managing symptoms and slowing disease progression has evolved into one where medications can significantly alter disease trajectories and improve outcomes across multiple measures.
For patients with heart disease, these advances mean more than just statistics – they represent the possibility of fewer hospitalizations, improved daily functioning, and longer lives. The integration of these medications into standard treatment protocols has already begun to change the face of cardiology practice worldwide.

New medications are helping heart patients lead fuller, more active lives
As research continues and more innovative treatments move from clinical trials to FDA approval, the future of heart care looks increasingly promising. The combination of these new medications with advances in diagnostic technologies, surgical techniques, and preventive strategies is creating a comprehensive approach to cardiovascular disease that offers hope to millions of patients worldwide.
Want to Learn if New Heart Medications Could Help You?
Your primary care provider or cardiologist can help determine if these innovative treatments are right for your specific condition. Schedule a consultation today to discuss your heart health and explore the latest treatment options.