AI-Powered Early Detection Tools
Artificial intelligence has revolutionized how we identify and diagnose heart conditions, often before symptoms become apparent. The integration of machine learning algorithms with traditional diagnostic tools has created powerful new systems capable of detecting subtle patterns invisible to the human eye.
Advanced Imaging Analysis
In 2025, AI-enhanced imaging has become the gold standard for cardiovascular diagnostics. These systems process ultrasound images, cardio sonograms, X-rays, CT scans, and MRIs with unprecedented precision. According to Dr. Yiannis Chatzizisis, professor in the Division of Cardiovascular Medicine at the University of Miami, “Today’s AI algorithms don’t just detect symptoms—they predict complications and guide personalized treatment strategies.”

Recent FDA approvals have accelerated the adoption of these technologies. The CardioVision AI platform, cleared in early 2025, demonstrated a 94% accuracy rate in identifying early-stage coronary artery disease—significantly higher than the 76% achieved by experienced cardiologists alone. This system now serves as both a diagnostic tool and a second opinion for physicians.
Wearable Monitoring Devices
The evolution of wearable technology has transformed from simple fitness trackers to sophisticated medical devices. Modern smartwatches and biosensors monitor heart rate, blood pressure, oxygen saturation, and even detect arrhythmias in real-time. These devices are now integrated with healthcare systems, allowing for continuous monitoring and early intervention.

Dr. Michael Dyal, assistant professor in cardiovascular medicine, notes that “The integration of AI with wearable technology has created an early warning system that has already prevented thousands of heart attacks and strokes. These devices don’t just collect data—they analyze patterns and alert both patients and physicians to concerning changes.”
“The future of cardiac diagnostics lies in gathering data through non-invasive monitoring, followed by AI-powered analysis and personalized treatment recommendations tailored to each patient’s unique cardiovascular profile.”
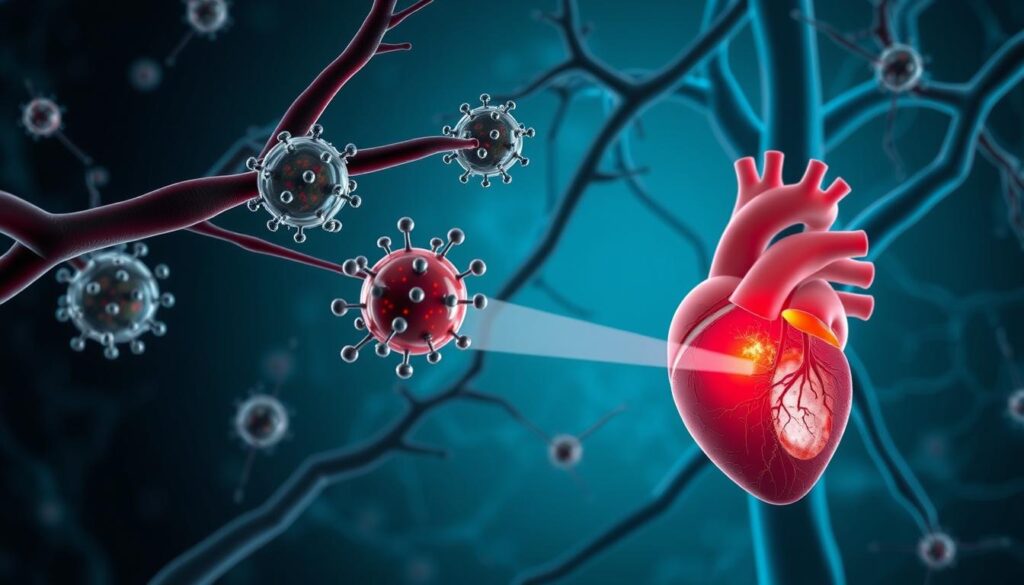
Nanotechnology in Artery Repair
One of the most exciting developments in heart disease treatment is the application of nanotechnology to repair damaged arteries and heart tissue. These microscopic tools are revolutionizing cardiovascular interventions with their precision and minimally invasive nature.
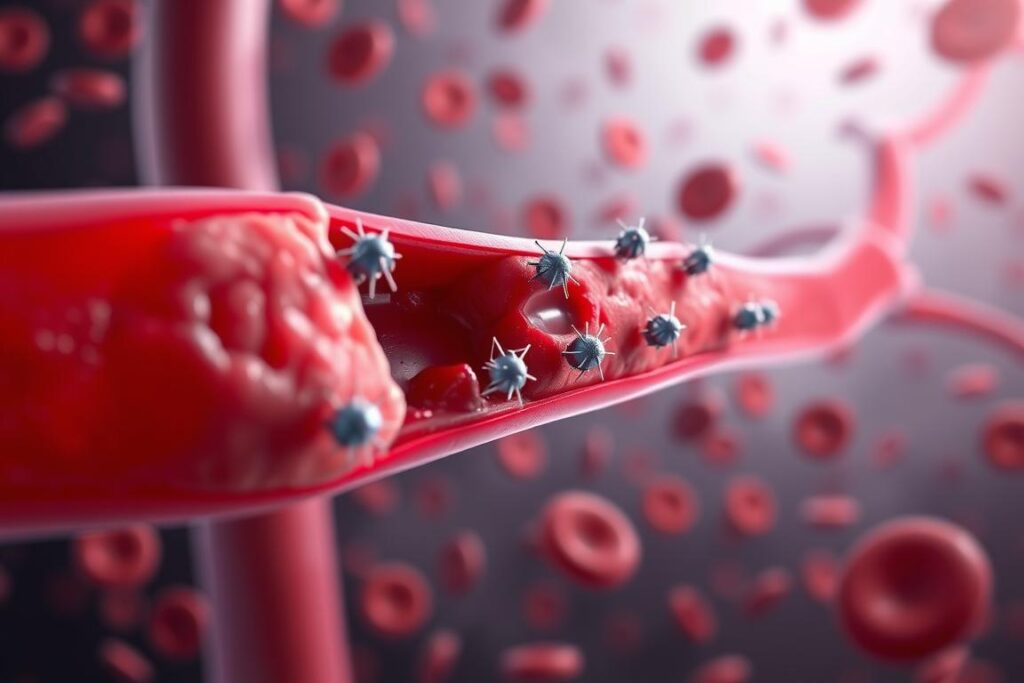
Targeted Drug Delivery
Nanoparticles engineered to deliver medications directly to inflammation sites in the heart have shown remarkable efficacy in clinical trials. These particles can navigate the bloodstream and release their therapeutic payload precisely where needed, minimizing side effects on the rest of the body.
The NanoHeart delivery system, approved in mid-2025, demonstrated a 78% improvement in medication efficacy compared to traditional delivery methods. Patients receiving targeted therapy for post-heart attack inflammation showed significantly better recovery rates and reduced scarring of heart tissue.
Endovascular Nanorobots
Perhaps the most futuristic application of nanotechnology is the development of nanorobots designed for endovascular operations. These microscopic machines can clear arterial blockages and repair tissue damage from inside the body without requiring major surgery.
While still in advanced clinical trials, preliminary results from the ArteryClear nanorobot system show promising outcomes. In a study of 150 patients with severe coronary artery disease, those receiving nanorobot treatment experienced a 65% reduction in blockage without the need for traditional stenting procedures.
Key Benefit: Nanotechnology interventions can target specific areas of cardiovascular damage with minimal impact on surrounding healthy tissue, potentially eliminating the need for invasive surgeries in many cases.
CRISPR-Based Therapies for Genetic Heart Risks
Gene editing technology has moved from science fiction to clinical reality, with CRISPR-Cas9 making significant breakthroughs in treating genetic heart conditions. These therapies address the root causes of certain cardiovascular diseases by modifying the genes responsible.
Treating Familial Hypercholesterolemia
One of the most successful applications of CRISPR in cardiology has been treating familial hypercholesterolemia, a genetic condition that causes dangerously high cholesterol levels and early heart disease. By altering the genes that influence cholesterol metabolism, researchers have achieved remarkable results.
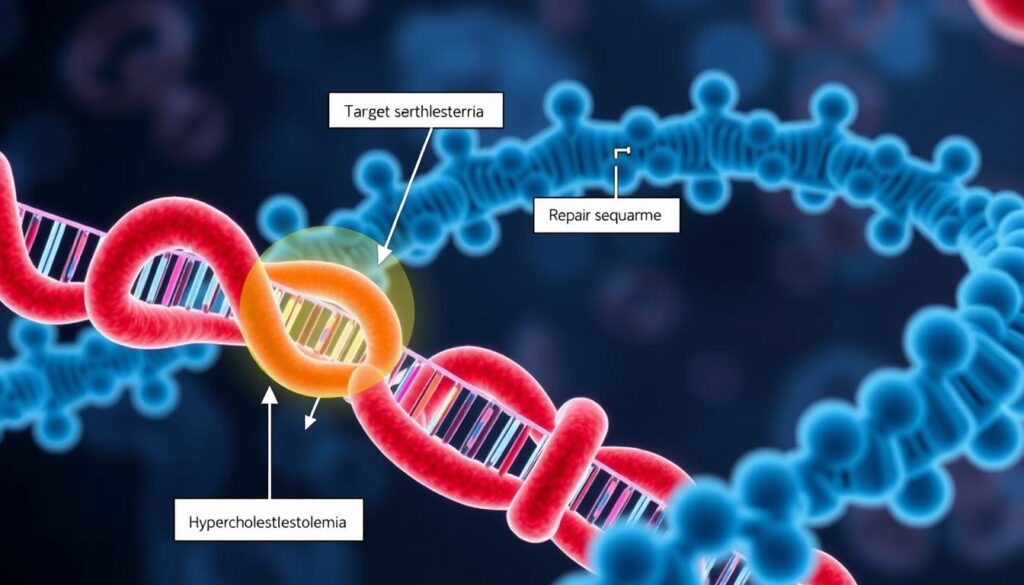
Clinical trials completed in early 2025 demonstrated that patients receiving CRISPR therapy experienced an average 62% reduction in LDL cholesterol levels, maintained for over 12 months after a single treatment. This represents a paradigm shift from daily medication to potential one-time curative therapy.
Preventing Heart Muscle Damage
Another promising application involves using CRISPR to prevent damage to heart muscle in patients who have suffered a heart attack. By editing genes involved in the inflammatory response, researchers can reduce scarring and promote healthier healing.
The MEND-Heart trial, which concluded in February 2025, showed that patients receiving gene editing therapy within 48 hours of a heart attack had 43% less permanent heart damage compared to the control group. This translated to significantly better heart function and quality of life during recovery.

Safety Note: While early results are promising, researchers continue to monitor for potential off-target effects. Current protocols include comprehensive genetic screening before treatment to ensure patient safety.
“CRISPR technology is allowing us to address the genetic roots of heart disease rather than just managing symptoms. This represents a fundamental shift in our approach to cardiovascular medicine.”
Smart Implants with Real-Time Monitoring
The integration of digital technology with implantable cardiac devices has created a new generation of “smart” implants that do far more than their predecessors. These devices not only provide therapeutic functions but also continuously monitor heart health and communicate with healthcare providers.
Advanced Pacemakers and Defibrillators
Traditional pacemakers and defibrillators have evolved into sophisticated systems capable of adapting to changing patient conditions. The latest models use machine learning to optimize their function based on individual patient patterns.

The CardioSync system, introduced in 2025, features AI-driven rhythm management that can predict and prevent up to 89% of dangerous arrhythmias before they occur. These devices also transmit comprehensive data to physicians, allowing for remote adjustments without requiring office visits.
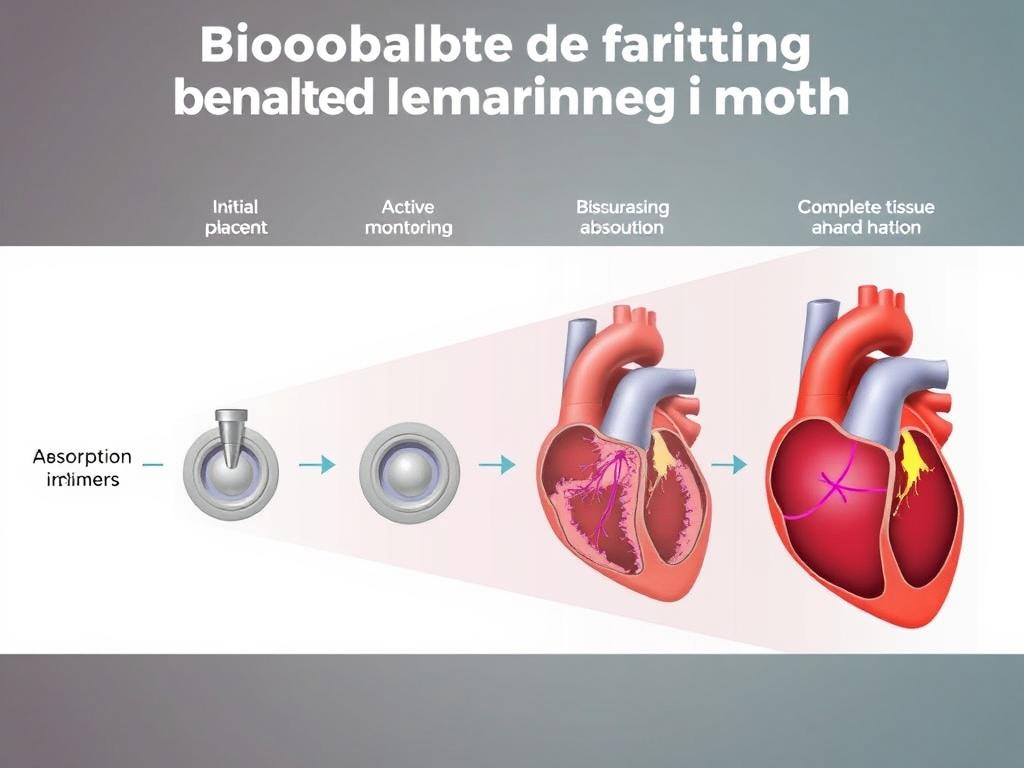
Bioresorbable Monitoring Implants
A groundbreaking development in cardiac monitoring is the creation of bioresorbable implants that dissolve naturally after serving their purpose. These temporary devices can be placed during recovery from heart procedures to provide detailed monitoring during the critical healing phase.
The HeartGuard temporary monitoring system, approved in January 2025, is implanted during cardiac procedures and provides continuous data for up to six months before harmlessly dissolving. Clinical studies show that patients with these monitors experienced 72% fewer complications during recovery due to early detection of potential issues.
Remote Monitoring Platforms
The data collected by these smart implants feeds into sophisticated remote monitoring platforms that use AI to analyze patterns and alert medical teams to concerning changes. This creates a continuous care model rather than the traditional episodic approach.
Dr. Raul Mitrani, director of clinical cardiac electrophysiology, explains: “These systems don’t just react to emergencies—they predict and prevent them. We’re now able to adjust medications or recommend interventions based on subtle changes in a patient’s data, often before they feel any symptoms.”
Hybrid Cardiac Rehabilitation Programs
The approach to cardiac rehabilitation has undergone significant transformation, with new hybrid models combining traditional in-person therapy with digital solutions. These programs recognize that recovery from heart disease requires both physical and psychological support.

Modern rehabilitation programs incorporate virtual reality environments to simulate exercise conditions, allowing patients to engage in guided therapy from home while being monitored remotely. These programs also address the mental health aspects of heart disease, integrating psychological support to manage depression and anxiety that often accompany cardiac conditions.
Studies of hybrid rehabilitation models show a 68% improvement in patient adherence compared to traditional programs, resulting in better long-term outcomes and reduced readmission rates. The flexibility of these approaches makes cardiac rehabilitation accessible to patients regardless of location or mobility limitations.
Traditional Rehabilitation
- Facility-based sessions only
- Limited schedule options
- Focus primarily on physical exercise
- Standard approach for all patients
- Minimal between-session monitoring
Hybrid Rehabilitation
- Combination of in-person and remote sessions
- Flexible scheduling to improve adherence
- Integrated physical and mental health support
- Personalized based on patient data
- Continuous monitoring via connected devices
The Future of Heart Disease Treatment
The innovations we’ve explored represent just the beginning of a new era in cardiovascular medicine. As we look toward the future, several trends are likely to shape the continued evolution of heart disease treatment:

- Personalized Medicine: Treatment plans tailored to individual genetic profiles, lifestyle factors, and specific heart conditions
- Preventive Focus: Shift from treating established disease to preventing its development through early intervention
- Integration of Technologies: Combining AI, nanotechnology, gene editing, and digital monitoring into comprehensive care systems
- Patient Empowerment: Greater involvement of patients in managing their heart health through accessible technology and education
While these innovations offer tremendous promise, it’s important to remember that the foundation of heart health still rests on prevention through lifestyle choices. Even the most advanced treatments cannot replace the value of a heart-healthy diet, regular exercise, stress management, and avoiding tobacco.
For those already diagnosed with heart disease, these new technologies offer hope for better outcomes and improved quality of life. The pace of innovation suggests that treatments considered experimental today may become standard care in the near future.
Take Control of Your Heart Health
The innovations in heart disease treatment are evolving rapidly. To learn if these cutting-edge approaches might benefit your specific condition, consult with a cardiologist specializing in advanced cardiovascular care. Early adoption of appropriate treatments can significantly improve outcomes.
“As we look forward, one thing is certain: the battle against heart disease is becoming smarter and more precise than ever before. These innovations don’t just treat heart disease—they’re transforming lives.”
Frequently Asked Questions About Heart Disease Treatment Innovations
Are these new heart disease treatments covered by insurance?
Coverage varies by treatment and insurance provider. Many established innovations like advanced imaging and certain smart implants are increasingly covered by major insurance plans. Newer technologies like CRISPR therapies and nanotechnology treatments may have limited coverage while they transition from experimental to standard care. Always check with your insurance provider and healthcare team about specific coverage for innovative treatments.
How do I know if I’m a candidate for these innovative treatments?
Candidacy depends on your specific heart condition, overall health, genetic factors, and treatment history. A cardiologist specializing in advanced cardiovascular care can evaluate your case and determine which innovations might benefit you. Many treatments require specific diagnostic tests to confirm eligibility, such as genetic screening for CRISPR therapies or detailed imaging for nanotechnology interventions.
What are the risks associated with these new treatments?
Each innovation carries its own risk profile. AI diagnostic tools have minimal direct risks but depend on accurate data interpretation. Nanotechnology and CRISPR therapies are more invasive and may have risks including immune reactions, off-target effects, or unforeseen long-term consequences. However, these technologies undergo rigorous safety testing before approval. Your healthcare provider should discuss specific risks and benefits for any recommended treatment.
How can I access clinical trials for these heart disease innovations?
To access clinical trials, start by discussing your interest with your cardiologist, who may know of relevant studies. You can also search the National Institutes of Health clinical trials database at ClinicalTrials.gov or contact major cardiac research centers directly. Patient advocacy organizations for specific heart conditions often share information about trial opportunities. Remember that trials have specific eligibility criteria that you must meet to participate.