The Biological Connection Between Diabetes and Heart Disease
How diabetes affects your cardiovascular system
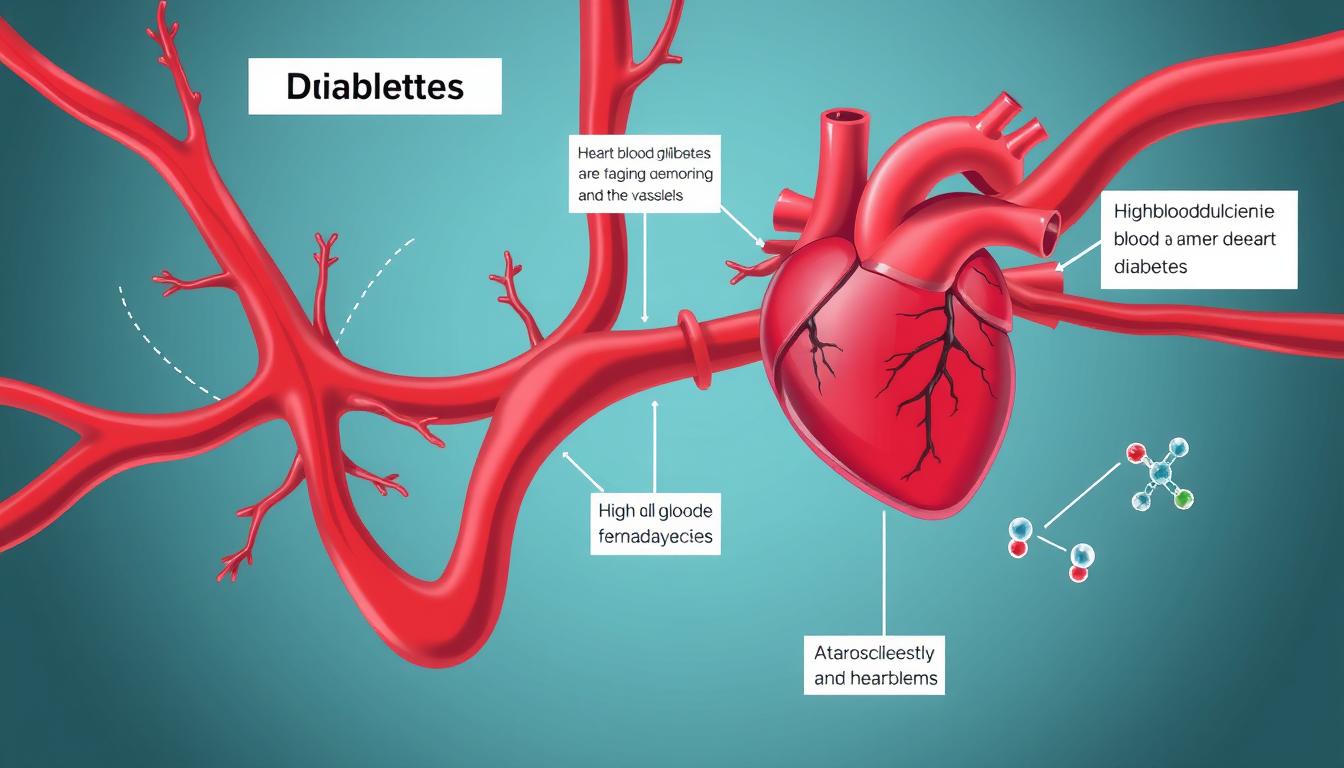
When you have diabetes, your body either doesn’t produce enough insulin (Type 1) or can’t effectively use the insulin it produces (Type 2). This leads to elevated blood glucose levels that can damage blood vessels and nerves throughout your body, including those that control your heart.
Type 1 Diabetes and Your Heart
In Type 1 diabetes, the immune system attacks insulin-producing cells in the pancreas. Without sufficient insulin, glucose builds up in the bloodstream instead of entering cells for energy. This chronic high blood sugar damages blood vessel linings and accelerates atherosclerosis—the buildup of fatty deposits in arteries—leading to reduced blood flow to the heart.
Type 2 Diabetes and Cardiovascular Risk
Insulin resistance, the hallmark of Type 2 diabetes, creates a perfect storm for heart problems. When cells resist insulin’s effects, the pancreas produces more insulin to compensate. This excess insulin, along with high blood glucose, triggers inflammation, blood vessel damage, and abnormal cholesterol metabolism—all contributing to heart disease.
“Having diabetes means you are more likely to develop heart disease. People with diabetes are also more likely to have certain risk factors that increase their chances of having a heart attack or stroke.”
According to the American Heart Association, adults with diabetes are nearly twice as likely to die from heart disease or stroke compared to people without diabetes. This stark statistic underscores the vital importance of understanding and managing both conditions simultaneously.
Key Risk Factors: When Diabetes and Heart Health Collide
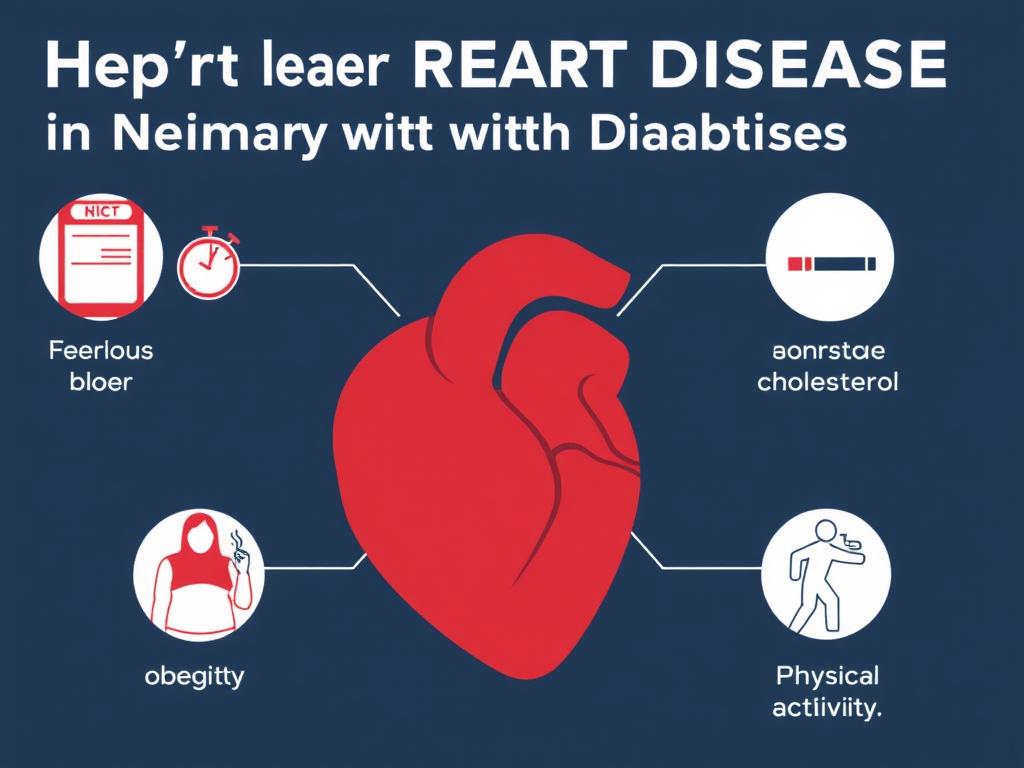
Several factors significantly increase your risk of developing heart disease when you have diabetes. Understanding these risk factors is the first step toward effective prevention and management.
High Blood Glucose
Persistently elevated blood sugar levels damage blood vessels and accelerate atherosclerosis. The American Diabetes Association recommends an A1C target of less than 7% for most adults with diabetes to reduce cardiovascular complications.
Hypertension
High blood pressure forces your heart to work harder to pump blood. When combined with diabetes, this significantly increases your risk of heart attack, stroke, and kidney problems. The target blood pressure for most people with diabetes is below 140/90 mmHg.
Cholesterol Imbalances
Diabetes often disrupts your cholesterol profile, increasing LDL (“bad”) cholesterol and triglycerides while decreasing HDL (“good”) cholesterol. This imbalance accelerates plaque buildup in arteries, restricting blood flow to your heart.
Obesity and Physical Inactivity
Excess weight, particularly around the waist, increases insulin resistance and puts additional strain on your heart. Physical inactivity compounds these risks by weakening your cardiovascular system and making weight management more difficult.
Did you know? Having excess belly fat significantly increases your heart disease risk. Your waist measurement should be less than 40 inches for men or 35 inches for women to reduce cardiovascular risk.
Additional Risk Factors
- Smoking: Tobacco use narrows blood vessels, raises blood pressure, and reduces oxygen in the blood—all particularly dangerous for people with diabetes.
- Family history: A family history of heart disease doubles your risk, making preventive measures even more crucial.
- Chronic kidney disease: About 40% of people with diabetes develop kidney problems, which further increase heart disease risk.
- Stress and depression: These conditions can make diabetes management more difficult and independently increase heart disease risk.
Prevention Strategies: Protecting Your Heart with Diabetes

Taking proactive steps to protect your heart is essential when you have diabetes. These prevention strategies can significantly reduce your risk of developing cardiovascular disease.
Know Your ABCs
| Measure | Target Goal | Why It Matters |
| A1C (Blood Glucose) | Below 7% for most adults | Reduces risk of blood vessel damage and heart complications |
| Blood Pressure | Below 140/90 mmHg | Decreases strain on heart and blood vessels |
| Cholesterol (LDL) | Below 100 mg/dL | Prevents plaque buildup in arteries |
| Smoking | Complete cessation | Improves blood flow and reduces inflammation |
Take Control of Your Heart Health Today
Speak with your healthcare provider about your personal ABC targets and develop a plan to reach them.
Heart-Healthy Nutrition
A balanced diet is crucial for managing both diabetes and heart health. The American Diabetes Association recommends following these nutritional guidelines:
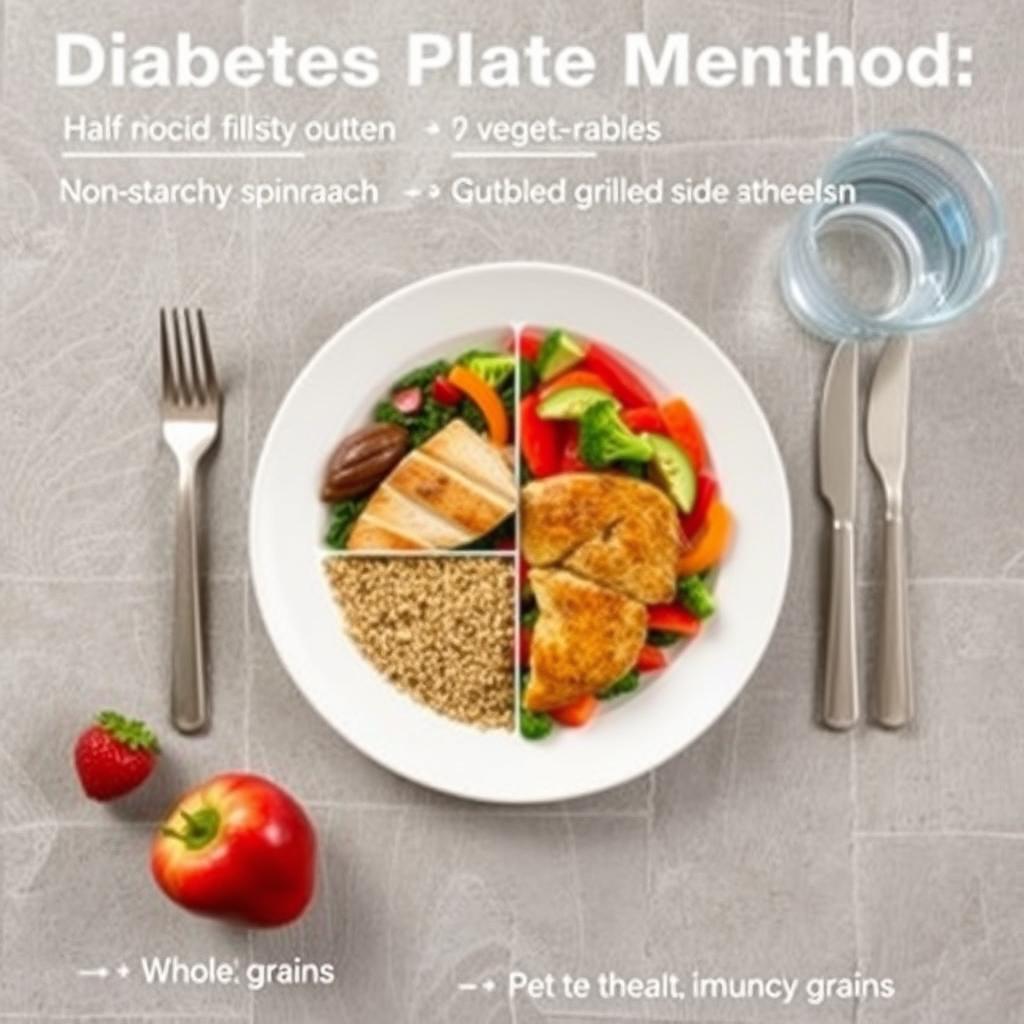
The Diabetes Plate Method for heart-healthy eating
Foods to Emphasize:
- Non-starchy vegetables (leafy greens, broccoli, peppers)
- Whole grains (brown rice, quinoa, whole wheat)
- Lean proteins (fish, poultry, legumes)
- Healthy fats (olive oil, avocados, nuts)
- Fresh fruits in moderation
Foods to Limit:
- Processed foods high in sodium
- Refined carbohydrates and added sugars
- Saturated and trans fats
- High-sodium foods
- Excessive alcohol consumption
Physical Activity for Heart Protection
Regular exercise improves insulin sensitivity, helps maintain healthy weight, strengthens your heart, and improves blood pressure and cholesterol levels. The American Heart Association and American Diabetes Association recommend:

- At least 150 minutes of moderate-intensity aerobic activity weekly (brisk walking, swimming, cycling)
- Resistance training 2-3 times per week to build muscle and improve insulin sensitivity
- Flexibility and balance exercises, especially for older adults
- Breaking up periods of sitting with light activity every 30 minutes
Start slowly and progress gradually. If you’ve been inactive, begin with just 5-10 minutes of walking daily and gradually increase duration and intensity as your fitness improves. Always consult your healthcare provider before starting a new exercise program.
Management Tips: Daily Actions for Diabetes and Heart Health

Effective daily management of both diabetes and heart health requires consistent attention and care. These practical tips can help you maintain control of both conditions.
Medication Adherence
Taking prescribed medications consistently is crucial for managing diabetes and protecting your heart. According to the World Health Organization, proper medication adherence can significantly reduce your risk of cardiovascular complications.
Diabetes Medications
Some diabetes medications offer additional heart benefits. For example, certain SGLT-2 inhibitors and GLP-1 receptor agonists have been shown to reduce cardiovascular events in people with type 2 diabetes and established heart disease.
Heart Medications
Many people with diabetes also benefit from medications to manage blood pressure, cholesterol, and reduce heart attack risk. These might include statins, ACE inhibitors, or low-dose aspirin (if recommended by your doctor).
Important: Never stop taking prescribed medications without consulting your healthcare provider, even if you feel better. Sudden discontinuation can lead to serious health consequences.
Regular Monitoring and Check-ups

Regular monitoring helps you catch potential problems early and adjust your management plan as needed. Establish a consistent schedule for:
- Blood glucose monitoring: Check your levels as recommended by your healthcare provider
- A1C tests: Every 3-6 months to assess long-term glucose control
- Blood pressure checks: At every medical appointment or more frequently if elevated
- Cholesterol screening: At least annually or as recommended
- Comprehensive foot exams: At least once yearly to check for circulation problems
- Eye examinations: Annual dilated eye exams to detect early vascular changes
- Kidney function tests: Annual screening for early detection of kidney disease
Stay on Track with Your Health
Create a personalized monitoring schedule with your healthcare team to protect your heart and manage your diabetes effectively.
Stress Management and Mental Health
Chronic stress can raise blood glucose levels and blood pressure, increasing heart disease risk. Prioritize stress management through:

- Regular physical activity
- Adequate sleep (7-8 hours nightly)
- Mindfulness and meditation
- Deep breathing exercises
- Social connection and support
- Professional mental health support when needed
Recognizing Warning Signs: When to Seek Help
Knowing the warning signs of heart problems can save your life. People with diabetes may experience atypical or subtle symptoms due to nerve damage. Be alert for:
Heart Attack Warning Signs
- Chest pain, pressure, or discomfort
- Pain radiating to arms, back, neck, or jaw
- Shortness of breath
- Cold sweat, nausea, or lightheadedness
- Unusual fatigue (especially in women)
Stroke Warning Signs (FAST)
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call emergency services
Call emergency services immediately if you experience these symptoms. Quick treatment can prevent permanent damage or death. Don’t wait to see if symptoms improve on their own.
Frequently Asked Questions About Diabetes and Heart Health

Can diabetes cause heart attacks?
Yes, diabetes significantly increases the risk of heart attacks. High blood glucose damages blood vessels and accelerates atherosclerosis (narrowing of arteries due to plaque buildup). People with diabetes are 2-4 times more likely to develop heart disease than those without diabetes. Additionally, diabetes often occurs alongside other cardiovascular risk factors like high blood pressure and abnormal cholesterol levels, creating a “perfect storm” for heart attacks.
How does exercise improve both diabetes and heart health?
Exercise delivers multiple benefits for both conditions:
- Improves insulin sensitivity, allowing your body to use insulin more effectively
- Helps maintain healthy weight and reduces abdominal fat
- Lowers blood pressure and improves cholesterol profiles
- Strengthens the heart muscle and improves circulation
- Reduces inflammation throughout the body
- Helps manage stress, which can affect both blood glucose and heart health
Even modest activity—like walking 30 minutes daily—can reduce cardiovascular risk by 30-40% in people with diabetes.
What foods should diabetics avoid for heart safety?
For optimal heart health with diabetes, limit or avoid:
- Processed foods: Often high in sodium, unhealthy fats, and refined carbohydrates
- Sugary beverages: Soda, sweetened tea, fruit juices, and sports drinks
- Refined carbohydrates: White bread, white rice, and low-fiber cereals
- Trans fats: Found in some processed foods and baked goods
- Saturated fats: Limit full-fat dairy, fatty meats, and tropical oils
- High-sodium foods: Processed meats, canned soups, and many restaurant meals
- Excessive alcohol: Limit to moderate consumption (one drink daily for women, two for men)
Instead, focus on vegetables, whole grains, lean proteins, healthy fats, and fresh fruits in appropriate portions.
Taking Control of Your Diabetes and Heart Health

The connection between diabetes and heart health is undeniable, but having diabetes doesn’t mean heart disease is inevitable. By understanding the risks and taking proactive steps to manage both conditions, you can significantly reduce your chances of developing cardiovascular complications.
Remember that small, consistent changes often yield the greatest results. Start with one or two manageable adjustments to your lifestyle, then gradually incorporate more heart-healthy habits as they become routine. Work closely with your healthcare team to develop a personalized plan that addresses your specific needs and risk factors.
With proper management, monitoring, and lifestyle modifications, you can live a long, active life while effectively controlling both your diabetes and protecting your heart health.
Start Your Heart-Healthy Journey Today
Take the first step toward better heart health by scheduling a comprehensive check-up with your healthcare provider to discuss your diabetes management and cardiovascular risk factors.