According to the American Heart Association, someone in the United States has a heart attack approximately every 40 seconds. Perhaps more alarming is that about 1 in 5 heart attacks occurs “silently” – with symptoms so mild or atypical that the person doesn’t realize what’s happening until the damage is discovered later.
Why Heart Attack Symptoms Differ Between Genders
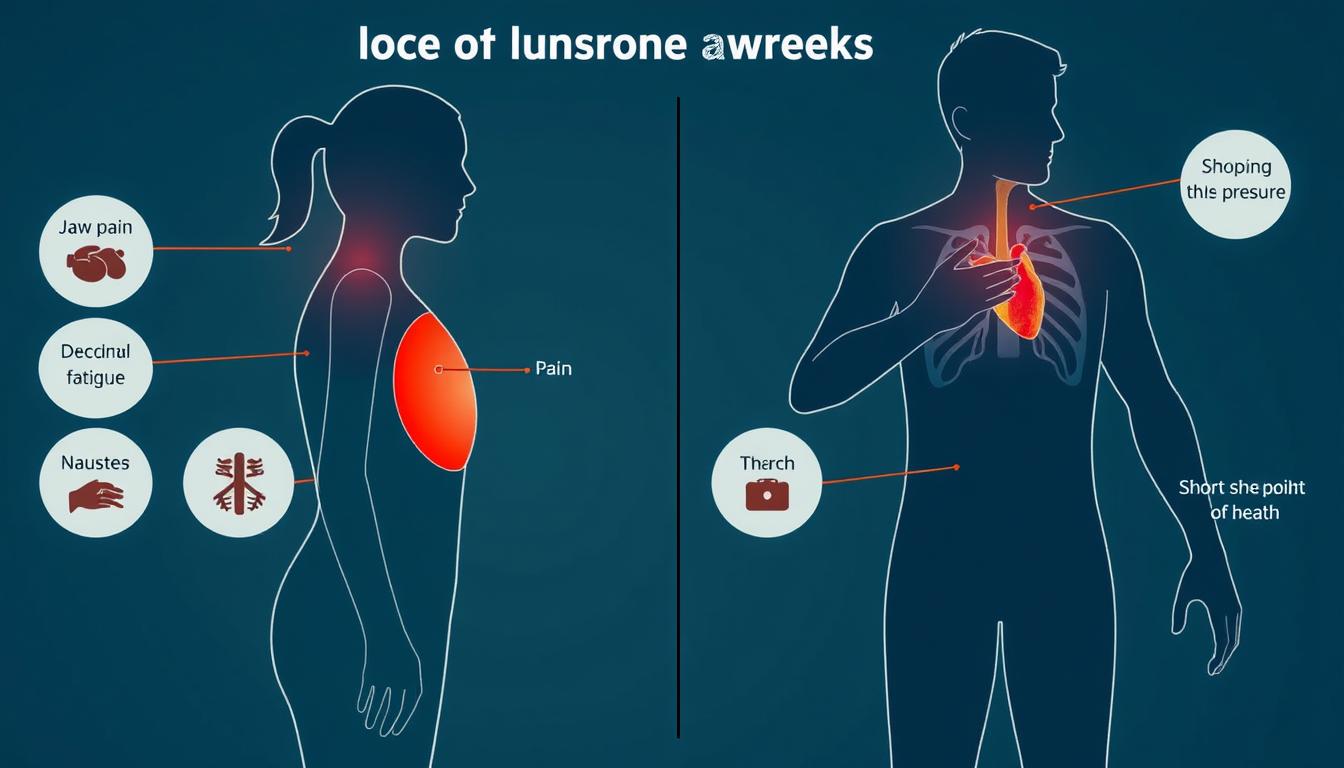
Heart attack symptoms can manifest differently in women and men due to biological and hormonal differences.
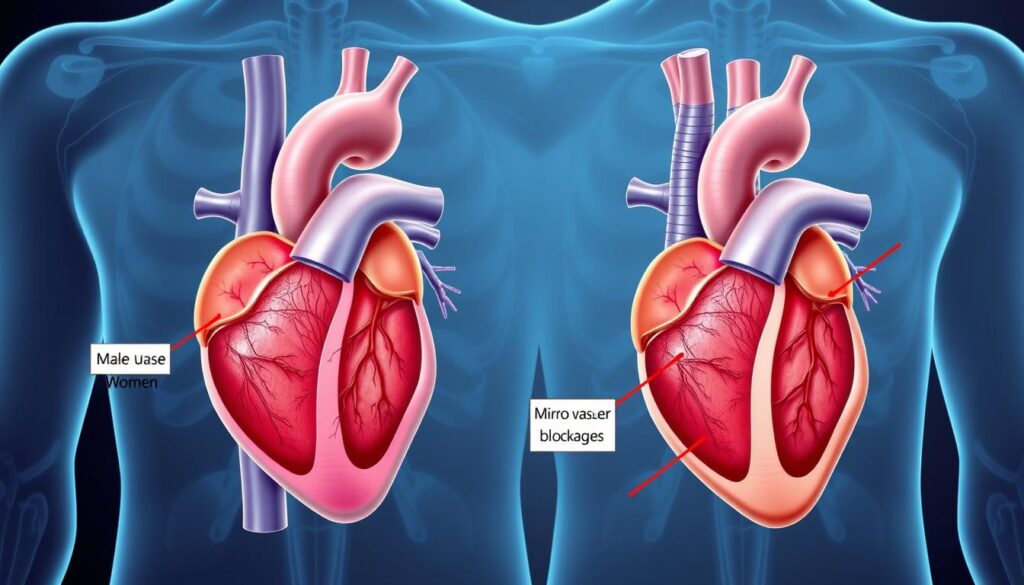
The way our bodies signal a heart attack isn’t one-size-fits-all. Biological differences, including hormonal variations, blood vessel size, and fat distribution patterns, contribute to how heart attacks manifest across genders.
Women often have smaller coronary arteries than men, and estrogen provides some heart protection until menopause. After menopause, women’s risk of heart disease increases dramatically. Additionally, women are more likely to experience coronary microvascular disease, which affects the tiny arteries around the heart rather than the major vessels.
These physiological differences help explain why women frequently experience more subtle, diffuse symptoms compared to the “classic” symptoms more commonly reported by men. Understanding these distinctions is crucial for prompt recognition and treatment.
Lesser-Known Heart Attack Symptoms in Women

Women often experience heart attacks differently than what’s portrayed in medical dramas. A study published in the Journal of the American Heart Association found that nearly 43% of women experienced no chest pain during their heart attack, making diagnosis challenging.
Unusual Symptoms to Watch For:
- Jaw, neck, or upper back pain: Pain that radiates to these areas, often described as pressure, aching, or tightness.
- Extreme fatigue: Overwhelming tiredness that persists for days or suddenly worsens, even with minimal activity.
- Unexplained nausea or vomiting: Digestive distress that occurs without obvious cause and may be dismissed as food poisoning or stomach virus.
- Shortness of breath without chest discomfort: Difficulty breathing that feels like you’ve run a marathon when you’ve only performed light activity.
- Lightheadedness or cold sweats: Sudden dizziness, clamminess, or breaking out in a cold sweat without exertion.
- Sleep disturbances: Research shows about 50% of women reported unusual sleep problems in the weeks before their heart attack.
Nearly 71% of women experienced unusual exhaustion in the weeks before their heart attack, according to studies from the National Institutes of Health.
Underrecognized Warning Signs in Men

While men more commonly experience the “classic” chest pain during a heart attack, they can also have subtle symptoms that get overlooked. These atypical signs deserve attention, especially in men with risk factors like high blood pressure, diabetes, or family history of heart disease.
Subtle Symptoms Men Often Dismiss:
- Persistent indigestion or heartburn: Discomfort that doesn’t respond to antacids and may be accompanied by a sensation of fullness or pressure.
- Unusual or excessive fatigue: Feeling exhausted after minimal exertion or experiencing a profound energy drop.
- Sleep disturbances: New onset of insomnia or waking up feeling unusually tired despite adequate sleep.
- Anxiety or sense of doom: An unexplained feeling that something is seriously wrong.
- Arm numbness or weakness: Not just the left arm (as commonly believed) but sometimes both arms or just the right arm.
- Subtle chest sensations: Rather than severe pain, some men report mild pressure, squeezing, or fullness that comes and goes.
Men are more likely to delay seeking medical attention for heart attack symptoms, with research showing an average delay of 3-4 hours compared to the recommended “golden hour” for treatment.
Why Symptoms Differ: Biological Factors
The biological underpinnings of symptom differences between women and men are complex and multifaceted. Understanding these factors helps explain why heart attacks can manifest so differently across genders.
Women-Specific Factors
- Microvascular disease: Women are more prone to blockages in the heart’s smaller blood vessels, which can cause different symptoms than blockages in main arteries.
- Hormonal influences: Estrogen provides some protection before menopause, but hormonal fluctuations can affect symptom presentation.
- Plaque erosion vs. rupture: Women more commonly experience plaque erosion rather than the rupture pattern seen in men.
Men-Specific Factors
- Larger coronary arteries: Men typically have larger main coronary arteries where blockages more often occur.
- Plaque composition: Men tend to develop harder, calcified plaque that ruptures suddenly.
- Autonomic nervous system: Differences in nerve pathways can affect how pain and discomfort are perceived and reported.
A study published in the Journal of the American Medical Association found that women under 55 are seven times more likely to be misdiagnosed and sent home during a heart attack compared to men of the same age. This alarming statistic underscores the importance of recognizing gender-specific symptoms.
Real-Life Scenarios: When Heart Attacks Don’t Follow the Script

“I thought I had a bad case of the flu. I was exhausted, nauseous, and had pain in my jaw and back. It never occurred to me I was having a heart attack because there was no chest pain.”
Case Study: The Marathon Runner
James, 48, was in excellent physical condition and ran marathons regularly. One evening after dinner, he felt mild indigestion and unusual fatigue. Thinking he was coming down with something, he went to bed early. The discomfort persisted through the night, accompanied by light sweating. Only when his arm began feeling numb did his wife insist on calling 911. At the hospital, doctors confirmed he was having a heart attack despite his excellent fitness level and absence of severe chest pain.
Case Study: The Busy Professional
Elena, 56, had been experiencing increasing fatigue for weeks. She attributed it to her demanding job and recent stress. One morning, she felt short of breath walking up the stairs and experienced unusual pressure between her shoulder blades. She took an antacid, thinking it was heartburn. When the symptoms didn’t improve after several hours, her colleague drove her to the emergency room. Tests revealed she was having a heart attack, though her symptoms never included the “classic” chest pain.
These cases illustrate how heart attacks often present with subtle, easily dismissed symptoms. Both individuals initially attributed their discomfort to common, less serious conditions—a dangerous but common mistake.
When to Seek Emergency Care

Knowing when to call 911 can be lifesaving. The American Heart Association emphasizes that minutes matter during a heart attack. The longer treatment is delayed, the more heart muscle can be damaged irreversibly.
Call 911 immediately if you experience any of these symptoms, especially if they are severe, come on suddenly, or don’t improve with rest:
- Chest discomfort (pressure, squeezing, fullness, or pain)
- Discomfort in other upper body areas (arms, back, neck, jaw, or stomach)
- Shortness of breath
- Cold sweat, nausea, or lightheadedness
- Extreme fatigue
- Anxiety or sense of doom
How to Describe Vague Symptoms to Healthcare Providers
When symptoms aren’t obvious, clearly communicating with medical professionals becomes crucial:
- Be specific about timing: “The discomfort began three hours ago and hasn’t improved.”
- Rate your discomfort: “On a scale of 1-10, my fatigue is an 8, which is unusual for me.”
- Describe sensations precisely: “It feels like pressure or squeezing rather than sharp pain.”
- Note pattern changes: “I’ve had heartburn before, but this feels different because it radiates to my jaw.”
- Mention risk factors: “I have diabetes and my mother had a heart attack at 60.”
Don’t Drive Yourself to the Hospital
Emergency medical services can begin treatment immediately upon arrival and notify the hospital to prepare for your arrival. This can save precious minutes when heart muscle is at risk.
Prevention and Symptom Awareness: Taking Control of Your Heart Health

While recognizing unusual heart attack symptoms is crucial, preventing heart disease altogether is the ultimate goal. A proactive approach to heart health can significantly reduce your risk of experiencing a heart attack.
Know Your Numbers
Regular check-ups with your healthcare provider can help monitor key indicators of heart health:
- Blood pressure: Aim for less than 120/80 mmHg
- Cholesterol: Target total cholesterol below 200 mg/dL
- Blood sugar: Fasting blood glucose under 100 mg/dL
- Body Mass Index (BMI): Maintain between 18.5-24.9
- Waist circumference: Less than 35 inches for women and 40 inches for men
Lifestyle Modifications That Save Lives
Heart-Healthy Diet
- Emphasize fruits, vegetables, and whole grains
- Choose lean proteins and plant-based options
- Limit saturated fats, trans fats, and sodium
- Reduce added sugars and processed foods
Regular Physical Activity
- Aim for 150 minutes of moderate exercise weekly
- Include both cardio and strength training
- Find activities you enjoy to maintain consistency
- Even short walks provide benefits
Take the First Step Toward Heart Health
Schedule a heart health assessment with your healthcare provider to identify your personal risk factors and develop a prevention plan tailored to your needs.
Surprising Statistics: The Impact of Delayed Diagnosis
The consequences of missing or delaying treatment for heart attack symptoms are significant and well-documented. Consider these eye-opening statistics:
| Statistic | Impact | Source |
| Women are 50% more likely than men to receive an incorrect initial diagnosis during a heart attack | Delayed treatment and increased risk of complications or death | Journal of the American Heart Association |
| For every 30-minute delay in treatment, the risk of dying increases by 7.5% | Emphasizes the critical importance of seeking immediate care | American College of Cardiology |
| Nearly 47% of sudden cardiac deaths occur outside a hospital | Suggests many people wait too long to seek medical attention | Centers for Disease Control and Prevention |
| People who experience “silent” heart attacks have a 3x higher risk of dying from heart disease | Highlights the danger of unrecognized symptoms | New England Journal of Medicine |
These statistics underscore the critical importance of recognizing unusual heart attack symptoms and seeking prompt medical attention. The data clearly shows that delays in diagnosis and treatment can have serious, sometimes fatal, consequences.
Recognizing the Signs Could Save Your Life

Heart attacks don’t always announce themselves with dramatic chest pain. For both women and men, the warning signs can be subtle, confusing, and easy to dismiss. Understanding the unusual symptoms that might indicate a heart attack could literally save your life or the life of someone you love.
Remember these key takeaways:
- Women and men often experience heart attacks differently due to biological factors
- Unusual fatigue, shortness of breath, and discomfort in the jaw, neck, or back can be warning signs
- Don’t dismiss symptoms as stress, indigestion, or normal aging
- When in doubt, check it out—calling 911 promptly can prevent permanent heart damage
- Know your personal risk factors and work with healthcare providers on prevention
“Time is muscle. The sooner you recognize symptoms and get treatment, the better your chances of recovery with minimal heart damage.”
Don’t Wait Until It’s Too Late
Learn your risk factors, recognize the warning signs, and have a plan in place for what to do if you experience potential heart attack symptoms.